Prevent Claim Denials in Medical Billing: Best Practices for 2024
Prevent Claim Denials in Medical Billing: Best Practices for 2024
Every denied medical claim isn’t just paperwork—it's a battle for persistence and financial stability in healthcare practices. Understanding the nuances of each claim submission is crucial to ensure prompt and full payment from insurance companies. However, issues like missing information or coding errors can lead to claim denials, directly impacting a practice's financial health.
In 2024, claim denials continue to pose significant challenges for healthcare organizations, with initial denial rates averaging close to 20% for received claims. For small to mid-sized practices, this can translate to a substantial loss of annual revenue, estimated at around 2% of net patient revenue.
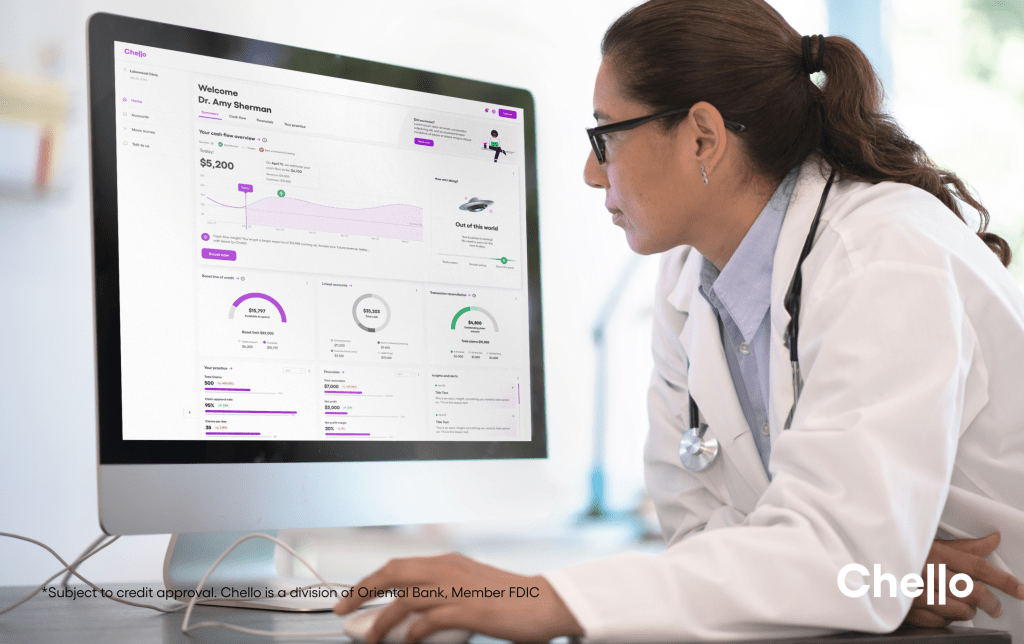
The ripple effect of claim denials extends beyond just administrative hurdles. It affects cash flow, impedes investment in growth opportunities, and demands additional time and resources for review, appeals, and refiling procedures.These expenses, both monetary and time-centered, are incurred solely to secure reimbursement for services provided—a challenging reality for any healthcare provider.
While achieving zero denials may not be feasible, reducing their frequency is attainable with a comprehensive denial management strategy. This strategy involves understanding the types of denials, addressing common reasons behind them, and implementing proactive measures to prevent their occurrence.
Types of Denials

Your private practice’s healthcare denials can fall into two categories: soft and hard denials. While both types result in claim rejection, they differ in terms of their nature and the potential for resolution. Let's explore the distinctions between hard denials and soft denials to gain a deeper understanding of their implications for healthcare providers.
Hard Denials:
- Hard denials are claim rejections that are typically non-negotiable and cannot be easily overturned or appealed.
- They occur when the insurance company determines that the claim does not meet the required criteria for reimbursement and denies it outright.
- Examples of hard denials include claims for non-covered services, duplicate claims, or claims submitted after the allowed time frame.
- Organizations usually have little recourse to challenge or appeal hard denials, and they result in a complete loss of reimbursement
Soft Denials:
- Soft denials are claim rejections that can be corrected or appealed with additional information or documentation.
- They occur when the insurance company identifies issues or errors in the claim but allows the provider to correct and resubmit the claim for reimbursement.
- Common reasons for soft denials include missing or incomplete information, coding errors, or insufficient documentation.
- Organizations can address the issues raised in the soft denial, make the necessary corrections, and resubmit the claim for reconsideration and potential reimbursement.
Common Reasons for Claim Denials

Claim denials can feel like hidden traps waiting to ensnare revenue streams of your practice. Understanding these pitfalls is essential for schedulers, providers, administrators, support staff, and the billing team alike. Although there could be any number of reasons for rejection, here are some of the most frequent to be on the lookout for.
1. Lack of Insurance Coverage
Keeping patient records up-to-date is an important first step in preventing this sort of denial. Asking patients when scheduling whether they have recently switched jobs or updated their insurance information can help. Asking for this information may seem like a nuisance but what could take a few seconds can prevent hours of frustration moving forward not to mention dollars saved.
2. Timely Filing
Each healthcare insurance provider is likely to have specific timeframes for when private practices should submit their claims. These can range from 15 days to potentially an entire year. Submitting late or missing any of these deadlines can result in having your claim denied. Generally, a patient cannot be sent a bill when a private practice has exceeded the deadline. It is important to stick to the dates on the calendar.
3. Inaccuracies in Coding:
Inaccuracies in medical coding for claims can have significant repercussions, often leading to denials and delays in reimbursement. These inaccuracies may arise from various sources, including human error, outdated codebooks, or insufficient documentation. Mistakes such as incorrect procedure or diagnosis codes, mismatched information, or failure to meet specific billing requirements can result in claim rejections by insurance companies or government payers.
4. Non-covered Services:
Denials for services not covered by insurance can happen for various reasons. Sometimes, the service isn't seen as medically necessary because of the diagnosis listed on the claim form. This might happen because the right diagnosis wasn't passed on to the billing team.
To avoid this, the coding and billing staff should know the common diagnoses linked to the services their providers offer. When they spot a service without the expected diagnosis, they can double-check with the provider's notes or ask the nursing staff for clarification.
4. Duplicate Claims:
Due to submitting duplicate claims occur when a healthcare provider accidentally or intentionally submits the same claim multiple times for the same service or procedure. This can happen due to various reasons such as system errors, misunderstandings in billing processes, or inefficiencies in communication among staff members.
Duplicate claims not only waste resources but also create administrative burdens for payers and delay the processing of legitimate claims. Healthcare providers should implement effective systems and checks to prevent the submission of duplicate claims, ensuring accurate and efficient billing practices while minimizing the risk of denials.
Best Strategies to Preventing Claim Denials

1.Implement comprehensive staff training programs focused on accurate coding and thorough documentation practices to minimize errors in claim submission.
2. Utilize advanced technology, such as claim scrubbing software (a tool used to automatically check claims for errors and inconsistencies before they are submitted to insurance companies), to identify and rectify errors before claims are sent, thereby reducing the likelihood of denials.
3. Establish clear and open communication channels between providers, billing staff, and payers to facilitate prompt resolution of issues and prevent misunderstandings that could lead to claim denials. Some suggestions to make this happen would be to schedule regular meetings and training sessions to discuss billing practices and updates, implementing procedures for obtaining pre-authorizations, or conducting regular audits to identify and address patterns leading to denials.
By understanding the common reasons behind claim denials and implementing effective strategies to combat them, healthcare practices can streamline their billing processes, optimize revenue cycle management, and improve overall financial performance.
Whether it's through comprehensive staff training, leveraging technology solutions, fostering open communication channels, or building strong relationships with payers, the key lies in proactive identification, prompt resolution, and ongoing monitoring of issues.
By taking these steps, healthcare providers can minimize claim denials, maximize reimbursement, and ultimately focus more time and resources on delivering quality patient care.